Maternal-fetal medicine (MFM) is an OB/GYN subspecialty. MFM doctors, also called perinatologists, are specialists in caring for and managing high-risk pregnancies.
Maternal-fetal medicine (MFM) is an OB/GYN subspecialty. MFM doctors, also called perinatologists, are specialists in caring for and managing high-risk pregnancies.
Many of the patients referred to Logan Health Maternal-Fetal Medicine have an uncomplicated pregnancy and are referred to the clinic for an advanced ultrasound examination, given our expertise in diagnosing fetal abnormalities and our ability to verify that the pregnancy is proceeding normally. Our OB/GYN providers, midwives and maternal-fetal specialists also care for high-risk pregnancies, where a pre-existing condition or a problem diagnosed in the pregnancy has put the mother or baby (sometimes both) at higher risk for complications.
We provide a multidisciplinary approach to high-risk pregnancies. Our patients are a part of our team, which includes your OB provider and other specialists as indicated. Logan Health has developed a core group of maternal and pediatric subspecialists, which allow us to care for any pregnancy or neonatal complication that can arise. Our goal is to identify at-risk pregnancies and reduce those risks through collaboration and planning
What we do
There are several different reasons someone may be referred to our clinic. These include:
Preconception Services
Our team offers preconception counseling for women with special pregnancy concerns. The team will help to create a personalized health plan for women who have:
- A history of pregnancy loss
- A history of preterm labor and/or delivery
- Chronic medical conditions (diabetes, thyroid disease, connective tissue disorders, hypertension and cardiac disease)
- Family or personal history of genetic disorders
- Advanced maternal age
Obstetrical Services
Our medical staff provide consultation and ongoing management through the various stages of high-risk pregnancies. They work with referring practitioners to optimize the prenatal care of women whose pregnancies are complicated by conditions such as:
- Diabetes
- Preterm labor
- Intrauterine growth restriction
- Disorders of amniotic fluid volume
- Hypertensive disorders
- Thyroid disease
- Cardiovascular disease
- Multiple gestation
- Incompetent cervix
High-Risk Deliveries
The providers at Logan Health Maternal-Fetal Medicine work with referring practitioners to coordinate care and make determinations regarding the labor management and delivery of women with high-risk needs. Although most patients who receive consultation and diagnostic services from Logan Health Maternal-Fetal Medicine deliver their baby with the aid of their general OB/GYN, our medical providers offer delivery care for a variety of high-risk scenarios such as:
- Transport to Logan Health Medical Center due to a need for a higher level of care
- Severity of risk high enough to warrant care by the perinatologist
- Preterm labor
- Emergency or scheduled C-section due to severe complications
Genetic Counseling
Prenatal diagnosis and genetic counseling are provided in a supportive manner for families at risk for fetal abnormalities or hereditary disorders due to such conditions as:
- Advanced maternal age
- Abnormal first or second trimester screen results
- Fetal anomalies detected by ultrasound
- Family or personal history of genetic disorders
- Medication, environmental or teratogen exposures
Ultrasound and Fetal Diagnosis
Logan Health Maternal-Fetal Medicine upholds the highest standards for practicing ultrasound, using modern imaging technology. Complete fetal anatomy and growth assessment scans are offered to detect many abnormalities. Our medical staff review every study and are available to report immediate results and develop a plan for patients and referring providers so there are no delays.
Pregnancy and Diabetes
Women who develop diabetes during pregnancy, which is also known as gestational diabetes, and women who have type 1 or type 2 diabetes prior to pregnancy (pregestational diabetes) face unique challenges. Diabetes in pregnancy may have serious health consequences for the mother and the baby during pregnancy and after delivery, but managing the disease can help prevent these complications.
At Logan Health, we provide highly specialized care for women with diabetes before, during, and after pregnancy. Our multidisciplinary team of experts, including maternal-fetal medicine specialists, endocrinologists, nurse practitioners, nutritionists, and social workers is dedicated to delivering the highest level of care and achieving healthy outcomes for pregnant women and their babies.
If I have diabetes, what should I do to prepare for pregnancy?
If you have type 1 or type 2 diabetes and are considering becoming pregnant, we recommend that you make an appointment with your primary care provider, a maternal-fetal medicine specialist and an endocrinologist and make sure that steps are in place to ensure a healthy pregnancy for yourself. These steps may include bringing your blood sugar control into a good range for pregnancy, making sure your medication regimen is safe for pregnancy, addressing any complications you may have, working on diabetes self-care, exercise and diet.
Maternal Transport
Medical transportation from facility to facility may be necessary in the right circumstances to offer a patient advanced medical care. Each patient is unique; however, our goal is to make the transfer to Logan Health easier and faster, so patients get the care they need, as soon as possible. Our emergency A.L.E.R.T. services support maternal transports and other critical care transfers.
Common Reasons for Maternal Transport
- Preterm labor
- Premature rupture of membranes
- Hypertensive disorders of pregnancy
- Insulin-dependent or gestational diabetes
- Vaginal bleeding
- Maternal medical complications
- Maternal obesity
- Multiple gestations
- Congenital abnormalities
- Anticipated neonatal intensive care for 22 weeks and greater gestations
How It Works
If you are interested in a maternal transport or consult, contact our transfer center at (844) 378-8701.
After providing a brief history you will be connected with one of our maternal fetal medicine physicians. Once transport is accepted, our maternal transport team will prepare for transport. Once en route, they will call with an estimated time of arrival.
After arrival, our team will introduce themselves, ask for a brief report and meet with the mom, family and providers to discuss a plan of care. Our maternal-fetal medicine physicians oversee all maternal transport activities.
Ultrasound FAQ
How long will my ultrasound take?
We allow 60 minutes for most ultrasound exams involving one fetus. If you are having a specialized test such as a fetal echocardiogram or Doppler studies, additional time will be scheduled. If you are scheduled for a consult with the maternal-fetal medicine specialist, additional time will be scheduled following the ultrasound.
For those who are new to Logan Health, arriving 15 minutes early helps us keep your appointment on track. This allows time for the perinatal nurse to take your vital signs and for you to fill out necessary forms. If you are bringing forms already completed, less advance time is necessary.
Do I need to have a full bladder?
Since sound waves do not travel well through bone, having a full bladder helps push a younger fetus up out of the bony pelvis for your pictures. Fluid in your bladder also provides a window for the sound to reach deeper structures and allows visualization of the birth canal.
We do not insist upon having a full bladder for your ultrasound. If you have had a normal fluid intake that day, during the course of the exam your bladder will fill. Once your pregnancy reaches approximately 30 weeks gestation, a full bladder is no longer helpful for ultrasound.
Will I hear my baby’s heartbeat?
Unless you are having a fetal echocardiogram or Doppler studies, it is not likely that you will hear the heartbeat. Your sonographer will document the heart rate in motion. You will see the motion of the heart beating and a graphical representation of heart motion over time. The baby’s heart rate is calculated from the graph.
Is ultrasound safe?
Ultrasound energy is different from radiation and has proven beneficial for use in imaging the fetus. The perinatal sonographer will keep the exposure level as low as possible by minimizing scanning time and keeping output settings on the ultrasound machine within an acceptable range. Although use of ultrasound is discouraged without medical necessity, it is considered safe when used by properly trained individuals.
What is transvaginal or vaginal ultrasound?
Transvaginal ultrasound is a valuable tool in certain instances. It provides a way to see deep or very small structures that might otherwise be covered up. It involves introducing a camera into the vagina and should not be painful. Typical reasons for using transvaginal ultrasound would be during early pregnancy and for measuring cervical length. Generally the sonographer will ask you to empty your bladder before the transvaginal ultrasound is performed.
Can ultrasound show Down syndrome or any other chromosome problems?
During the ultrasound, the sonographer will attempt to obtain images that provide in-depth information about fetal development. Often Down syndrome and other chromosome problems will be accompanied by abnormalities or findings that can alert the maternal-fetal medicine specialist.
Although an entirely normal ultrasound is reassuring and can lower the likelihood, it does not guarantee against the possibility of Down syndrome. An ultrasound is considered a screening test. In certain situations a more definitive test can be offered.
What can I expect to see when I have an ultrasound during the first trimester?
Due to advances in ultrasound technology it is now possible to see many of the early developing anatomical structures. As the fetus grows, more structures become visible. Although a first trimester scan does not replace the ultrasound anatomical survey generally done midway through the pregnancy, it can be very reassuring.
Ultrasound provides information that is used for some of the first trimester genetic screening tests, most commonly the nuchal translucency measurement. Every fetus has a narrow collection of fluid along the back of the neck, just under the skin, called the nuchal translucency. Measuring this fluid collection can be helpful in determining the risk of having a pregnancy affected by Down syndrome or another chromosome problem or syndrome. An abnormally thick nuchal translucency also may point to potential problems that can be checked for later in the pregnancy. Feel free to ask your provider about first trimester genetic screening options.
When can I find out if I am having a boy or girl?
Most patients find out midway through the pregnancy when they have an ultrasound for fetal development – called the anatomy survey, or anatomical survey. Some patients find out sooner if they have specialized genetic testing involving blood work or amniotic fluid sampling that gives them the sex information along with their genetic results. There is still some uncertainty about the accuracy of ultrasound information before 15-16 weeks gestation.
How big is my baby?
Ultrasound can start to show an embryo at about five to six weeks from the first day of your last period, when it measures 4-5 millimeters in length. By the end of the first trimester (we use 14 weeks as the upper range), the fetus measures approximately 3 inches from its bottom to the top of its head – the crown to rump length. Measurement of the crown to rump beyond the first trimester becomes increasingly unreliable due to positional differences from baby to baby – some curled up, some stretched out.
In the second and third trimesters, ultrasound begins to measure the head (diameter and circumference), abdomen (circumference) and femur (length). This is why a specific length is not given; instead we use an estimate of the weight based on a formula using these three measurements. Ultrasound estimation of fetal weight is clearly that – an estimation. At the midpoint of your pregnancy, the fetus generally weighs 12-14 ounces. During the third trimester, a general guideline for fetal weight gain is roughly a half pound per week.
What is a biophysical profile?
Ultrasound can be used to assist your provider in monitoring fetal well-being. A biophysical profile can be used as a standalone test or in conjunction with other types of monitoring such as nonstress testing.
A biophysical profile is a timed test that can last up to 30 minutes. The sonographer observes the fetus and environment while assigning a score based on the following:
- Limb body movements – at least three within the testing interval
- Fetal tone – flexion and extension
- Fetal breathing movements – 30 seconds of diaphragm motion
- Amniotic fluid – at least one pocket of fluid that measures a minimum of 2 centimeters deep by 1 centimeter wide
In addition, the sonographer often assesses blood flow through the umbilical cord, which gives your provider information about how the placenta is functioning.
During the scanning process the sonographer often records images to document the position of the fetus, placenta and some of the fetal organs.
3D Ultrasound
3D ultrasound is a newer technology made popular by the media’s use of the 3D baby face. 3D ultrasound actually has many other useful applications as well as some limitations. Logan Health uses 3D ultrasound whenever possible, depending on the position of your child and the medical benefit derived.
Meadowlark Initiative
What is the Meadowlark Initiative?
 The Meadowlark Initiative brings together medical care, counseling, care coordination and community services to help you get the right care at the right time, stay healthy and plan a path to recovery that works for you if you have concerns about depression, anxiety, drug and alcohol use, or other common stressors with the intention to help reduce the risk of pregnancy complications, and lastly, keep your family healthy, happy and together.
The Meadowlark Initiative brings together medical care, counseling, care coordination and community services to help you get the right care at the right time, stay healthy and plan a path to recovery that works for you if you have concerns about depression, anxiety, drug and alcohol use, or other common stressors with the intention to help reduce the risk of pregnancy complications, and lastly, keep your family healthy, happy and together.
You and your family receive individualized pregnancy care from an experienced, supportive clinical team. This team includes prenatal care providers (obstetricians, midwives and perinatologists), a behavioral health provider and a care coordinator. The behavioral health provider assesses referred patients and provides brief counseling intervention, outpatient therapy and referrals to other community-based counselors.
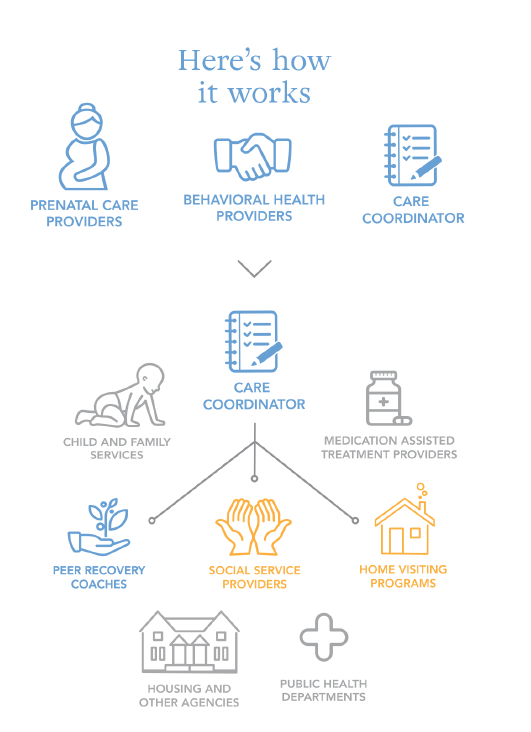
The care coordinator helps identify social factors that impede prenatal care and provide resources to meet those needs. This may include referrals to housing support, food stability agencies, substance use treatment, public health, home visiting programs, child care, medical coverage and employment agencies.
Contact Us
For more information about this initiative, contact Kalli Jacquay.
kjacquay@logan.org | (406) 758-1386
Meet Our Team
Contact Us
210 Sunnyview Lane, Suite 103
Kalispell, MT 59901
Phone and Fax
Phone: (406) 257-3872
Fax: (406) 758-7077
Office Hours
Monday, Wednesday, Thursday 7:30 a.m. to 5 p.m.
Tuesday 7:30 a.m. to 5 p.m.
Friday 7:30 a.m. to 12 p.m.
If you have any comments, questions or concerns, please don’t hesitate to contact our office
Patient Information
Click on the link below to review Logan Health’s notice of privacy practices, patient consent and financial agreement, advance directives, patient rights and responsibilities, organizational code of ethics, messages from Medicare and Tricare, and truth in lending.
Patient Rights and Policies